


- Stock: In Stock
- Package: 1mg/vial+water
Ask a Question About This Product
Long arginine 3-IGF-1, abbreviated as IGF-1 LR3 or LR3-IGF-1, is a synthetic protein and lengthened analogue of human insulin-like growth factor 1 (IGF-1).
WHAT IS IGF-1?
Insulin-like Growth Factor 1 (IGF-1) is a vital protein that plays an integral role in human growth and development. This recombinant human protein, which belongs to the insulin-like growth factor family, consists of 70 amino acids and functions similarly to insulin. It is involved in the regulation of various bodily processes, including cell growth, development, and differentiation, through endocrine, autocrine, and paracrine pathways.
One of the intriguing aspects of IGF-1 is its connection to aging. Research suggests that mutations in the IGF-1 gene can increase lifespan in laboratory animals, highlighting its potential impact on longevity. In children, IGF-1 is essential for stimulating cell growth and differentiation, while in adults, it continues to exert anabolic effects, promoting tissue growth and maintenance.
IGF-1 operates within a complex network of growth factors, receptors, and binding proteins that mediate cell proliferation, differentiation, and apoptosis. These growth factors are low-molecular-weight proteins present in nearly all tissues, where they regulate cell division, growth, and migration. In the skin, for instance, they are crucial for the migration and development of epithelial cells and stimulate cell division.
Often referred to as somatomedin C, IGF-1 serves as a key mediator of the growth hormone (HGH) effects. It is primarily produced by liver hepatocytes in response to growth hormone stimulation. The liver’s production of IGF-1 is influenced by various hormones, including sex steroids, thyroid hormones, glucocorticoids, and insulin. Insulin, androgens, and estrogens tend to enhance IGF-1 secretion, whereas glucocorticoids inhibit it. This interplay explains the synergy between these hormones in growth and development processes and the inhibitory impact of glucocorticoids on growth and puberty.
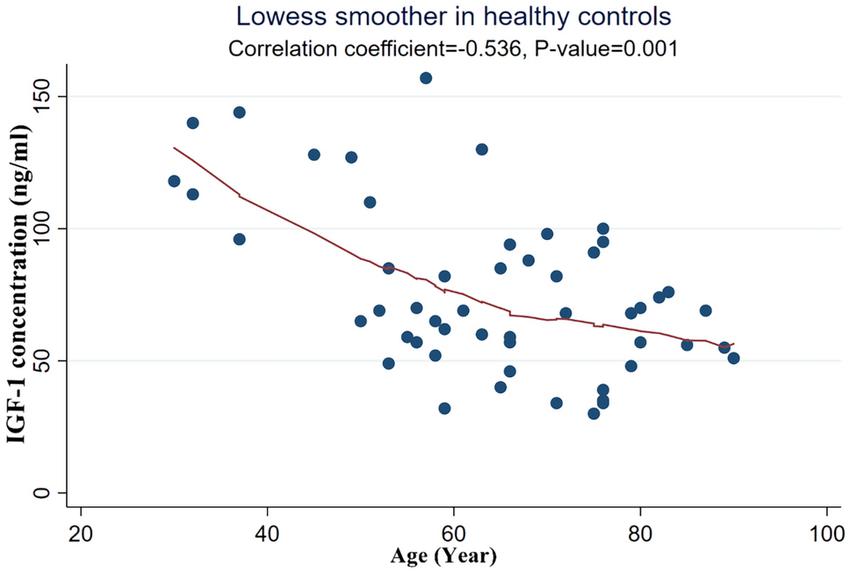
Throughout life, IGF-1 levels fluctuate, peaking during adolescence and dipping during childhood and old age. Despite these variations, IGF-1 remains a crucial anabolic hormone. It is secreted by various tissues, with the liver being the primary source, releasing IGF-1 into the bloodstream to act as an endocrine hormone. Other tissues, including cartilage cells, also secrete IGF-1, where it functions locally as a paracrine hormone.
In recent years, IGF-1 has garnered attention in the sports world as a doping agent, featuring in numerous high-profile doping cases. Its ability to enhance growth and performance makes it a substance of interest and concern in athletic communities.
WHAT IS THE DIFFERENCE BETWEEN IGF-1 AND IGF-1 LR3?
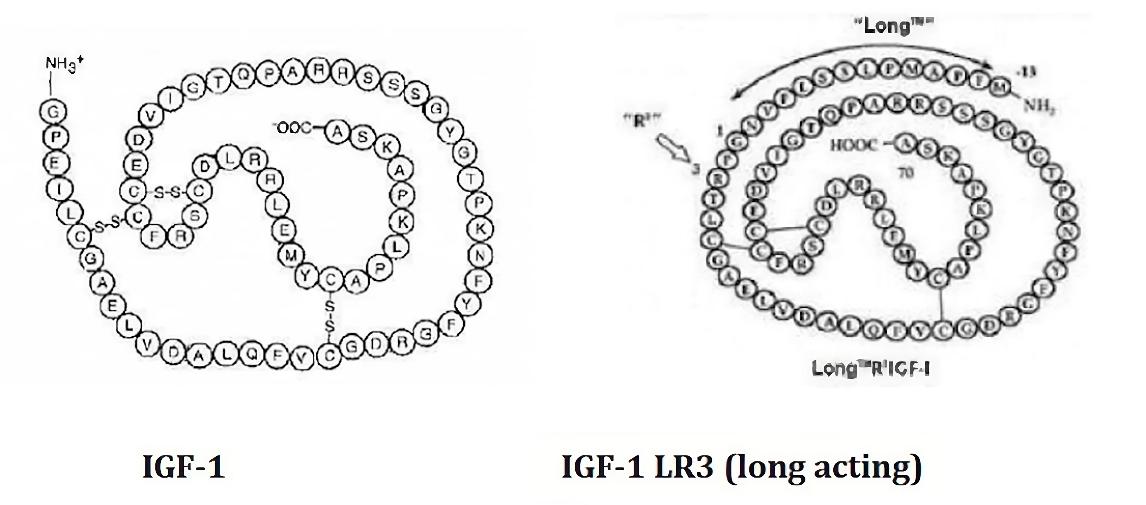
Insulin-like Growth Factor 1 (IGF-1) and its extended variant, IGF-1 LR3, share many similarities but also exhibit distinct differences that impact their functions and applications. IGF-1 is a naturally occurring protein in the human body, crucial for cell growth, development, and differentiation. It consists of 70 amino acids and acts by binding to IGF-1 receptors, influencing various physiological processes.
IGF-1 LR3, on the other hand, is a modified form of IGF-1, engineered to have a longer half-life and enhanced stability. This variant includes an additional 13 amino acids at the N-terminus, replacing the original third amino acid, glutamic acid, with an arginine. This modification significantly reduces IGF-1 LR3's binding affinity to IGF binding proteins, which typically regulate IGF-1's availability and activity. As a result, IGF-1 LR3 remains active in the bloodstream for a longer period, enhancing its efficacy in promoting growth and anabolic processes.
The extended half-life of IGF-1 LR3 makes it particularly valuable in both medical and athletic contexts. In medical settings, it offers potential therapeutic benefits for conditions requiring prolonged IGF-1 activity, such as muscle wasting diseases and growth deficiencies. In sports and bodybuilding, its prolonged action and potent anabolic effects make it a sought-after agent for enhancing muscle growth and performance. However, this also raises concerns about its misuse and the ethical implications in competitive sports.
In summary, while both IGF-1 and IGF-1 LR3 play vital roles in growth and development, the key difference lies in IGF-1 LR3's engineered structure, which confers a longer half-life and greater potency. This distinction not only expands its potential therapeutic applications but also underscores the need for careful regulation to prevent abuse in athletic environments.
MAIN EFFECTS
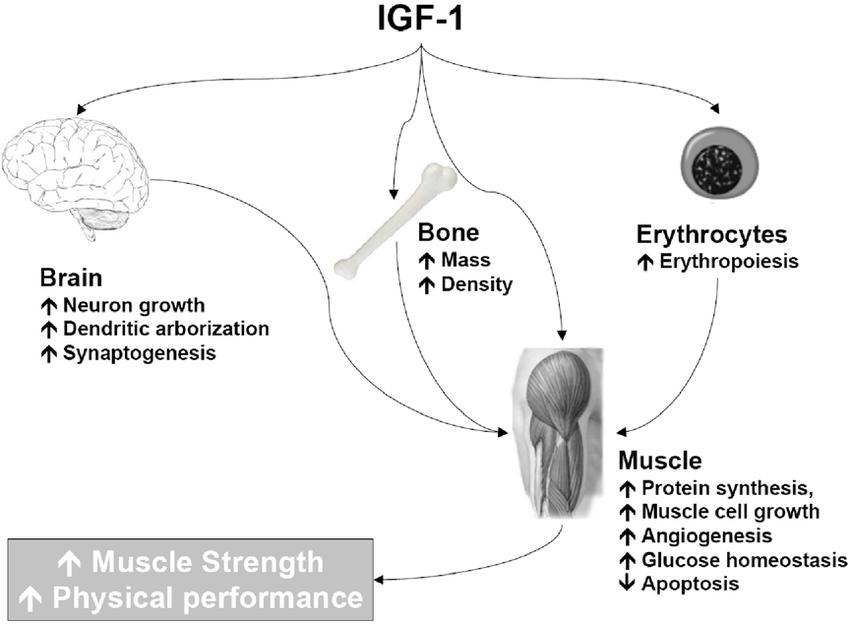
IGF-1 is an extremely powerful anabolic, which in combination with anabolic steroids gives a very large increase in lean muscle mass. At the same time, IGF-1 has a lot of other useful properties that together create the maximum boost for growth. IGF-1 is a product that can increase your result when other methods no longer give a significant effect.
Anabolic effects
- Increase in muscle mass (various ways of exposure)
- Muscle hyperplasia (unique property of increasing the number of muscle cells)
- Accelerated protein synthesis
- Regeneration of tendon tissue (increases collagen synthesis)
- Has a restorative effect on cartilage tissue
- Increases the effectiveness of anabolic steroids (increases the number of androgen receptors)
- Restores and strengthens bone and cartilage tissue
Support of the cardiovascular system
- Improves cardiac output, stroke volume, contractility and ejection fraction.
- Stimulates contractility and tissue remodeling in humans to improve heart function after myocardial infarction.
- Improves lipid profile
- Reduces insulin levels, increases insulin sensitivity and promotes glucose metabolism
- Reducing the overall risk of cardiovascular complications
- Helps fight inflammatory processes
Nerve tissue
- Increases glucose transport in nervous tissue
- Protects neurons at low glucose levels, preventing cell destruction.
- Play an important role in the restoration of neurons and nervous tissue in general
Other effects
- Regulate the expression of genes that increase life expectancy.
- Accelerates the restoration of the skin, prevents skin aging
- Improved immunity
Mechanism of action
Insulin-like growth factor-1 (IGF-1) is a vital protein that plays a crucial role in the regeneration and repair of various tissues in the human body, including bone, muscle, skin, and cartilage. When IGF-1 interacts with bone and cartilage tissue, it binds to specific receptors on osteoblasts and chondroblasts—cells responsible for the growth and repair of bones and cartilage. This binding stimulates these cells' metabolic activity, leading to accelerated healing of fractures and other bone injuries. IGF-1 also reduces inflammation in the damaged areas, enhancing the activity of cells involved in tissue renewal (Yakar et al., 2019).
Furthermore, IGF-1's metabolic effects extend beyond growth and repair. It plays a significant role in nutrient signaling, coordinating protein, fat, and carbohydrate metabolism across various cell types. This is achieved through the stimulation of IGF-1 receptors, which signal cells about the availability of nutrients. This coordination helps ensure that cells receive the necessary nutrients for growth and maintenance. Like insulin, IGF-1 is regulated by nutritional status and participates in glucose homeostasis. It lowers blood glucose levels by increasing glucose uptake in cells and reducing insulin secretion, which enhances insulin sensitivity (Samani et al., 2007).
In addition to its role in metabolism, IGF-1 also affects protein metabolism and lipolysis. It works synergistically with growth hormone (GH) to enhance the breakdown of fats and promote ketogenesis. This synergy between IGF-1 and GH is crucial for maintaining energy balance and supporting growth processes. Studies have shown that low levels of IGF-1 are often associated with metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes. This highlights the importance of IGF-1 in maintaining overall metabolic health (Clemmons, 2004).
Effects on Muscles
IGF-1 has a profound impact on muscle tissue, promoting muscle growth and repair. This is primarily achieved through the stimulation of satellite cells, which are stem cells located in the muscle tissue. When muscle tissue is damaged, IGF-1 activates these satellite cells, causing them to multiply and differentiate into new muscle cells. This process not only repairs damaged muscle fibers but also leads to an increase in muscle mass. IGF-1's ability to enhance muscle regeneration makes it a key treatment for conditions involving muscle atrophy, such as muscular dystrophy (Ahmad et al., 2020).
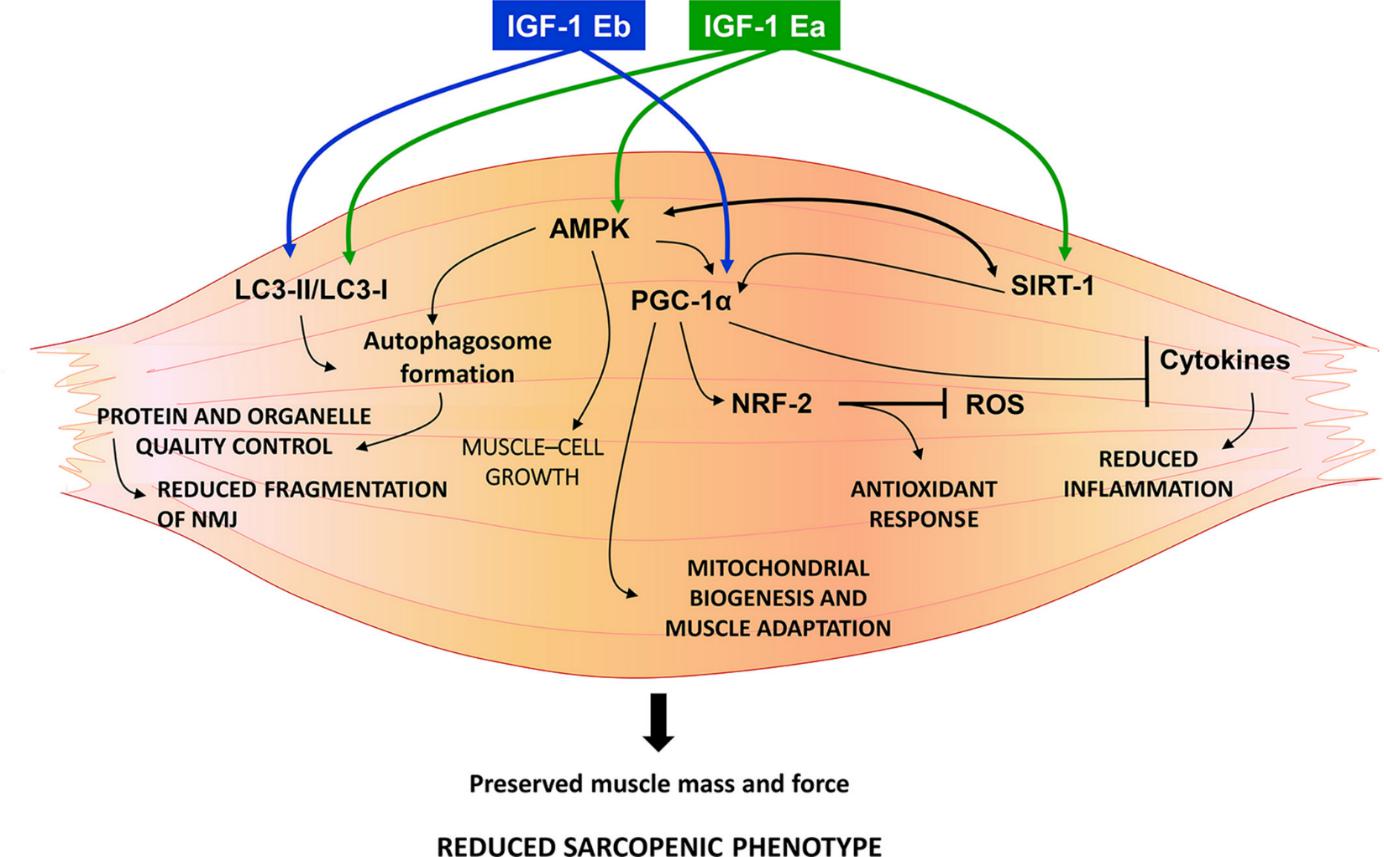
The molecular mechanisms by which IGF-1 stimulates muscle growth involve several signaling pathways. One of the primary pathways is the PI-3 kinase pathway, which leads to the activation of protein kinase B (AKT). AKT then promotes protein synthesis by activating the mTOR pathway, a crucial regulator of cell growth and protein synthesis. Additionally, IGF-1 enhances amino acid transport into muscle cells, providing the necessary building blocks for protein synthesis. IGF-1 also inhibits protein breakdown by downregulating the expression of genes involved in muscle atrophy, such as MuRF1 and MAFbx (Lai et al., 2004).
In addition to its anabolic effects, IGF-1 also has anti-catabolic properties. It counteracts the effects of inflammatory cytokines that promote muscle degradation. By inhibiting these catabolic pathways, IGF-1 helps preserve muscle mass and function, even in conditions of stress or disease. This dual role of promoting muscle growth and preventing muscle breakdown makes IGF-1 an essential factor in maintaining muscle health and function (Lai et al., 2004).
Effects on Tendon Tissue
Tendon injuries are notoriously slow to heal, often resulting in fibrovascular scarring that impairs the mechanical properties of the tendons and increases the risk of re-injury. IGF-1 has been shown to significantly enhance tendon healing by promoting cell proliferation, DNA synthesis, and matrix production, particularly collagen I, which is the primary component of tendon tissue. This makes IGF-1 a potent anabolic agent for improving tendon repair and function (Miescher et al., 2023).
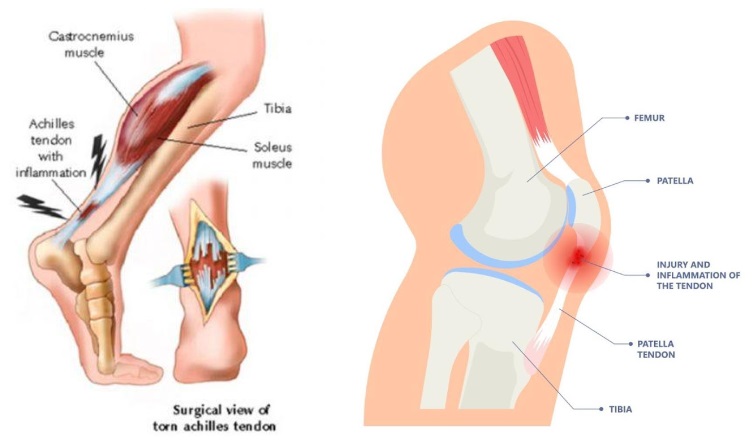
The mechanism by which IGF-1 promotes tendon healing involves several cellular processes. When applied to tenocyte cultures—cells that make up the tendons—IGF-1 stimulates these cells to proliferate and produce more extracellular matrix components, including collagen. This enhanced matrix production provides the structural support needed for tendon repair.Additionally, IGF-1 has been shown to reduce inflammation in the injured tendon, which further supports the healing process by creating a more favorable environment for tissue regeneration (Disser et al., 2019).
In preclinical animal models and human patients, IGF-1 has demonstrated its effectiveness in improving tendon healing outcomes. For instance, studies have shown that applying IGF-1 to injured tendons in animal models accelerates the healing process, reduces scarring, and improves the mechanical properties of the healed tendons. These findings suggest that IGF-1 could be a valuable therapeutic agent for treating tendon injuries in clinical settings. (Doessing et al., 2010)
Effects on Cartilage Tissue
IGF-1 plays a crucial role in the maintenance and repair of cartilage tissue, which is essential for joint health and function. Cartilage is a resilient and smooth elastic tissue that covers and protects the ends of long bones at the joints. It also serves as a cushion between bones, allowing smooth and pain-free movement. IGF-1 regulates cartilage metabolism by promoting anabolic processes and inhibiting catabolic processes, thereby maintaining cartilage integrity and function (Wen et al., 2021).
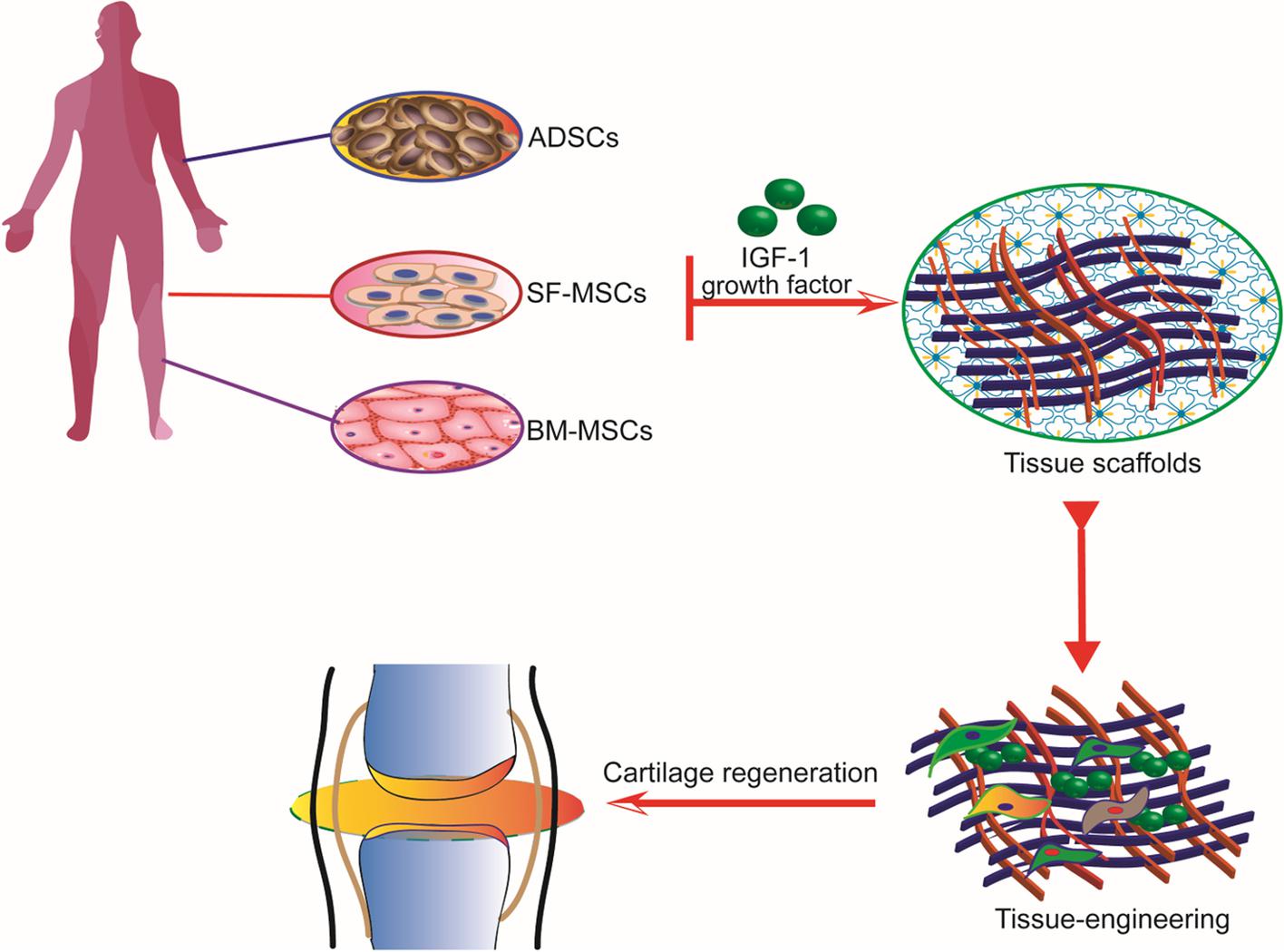
The primary cells responsible for maintaining cartilage are chondrocytes. IGF-1 stimulates these cells to produce extracellular matrix components, such as collagen and proteoglycans, which are essential for cartilage structure and function. In addition to promoting matrix synthesis, IGF-1 inhibits the activity of enzymes that break down cartilage, such as matrix metalloproteinases (MMPs). This dual action of promoting anabolic processes and inhibiting catabolic processes helps preserve cartilage tissue and prevent degeneration (Vedadghavami, 2022).
Studies have shown that IGF-1 can slow the progression of osteoarthritis, a degenerative joint disease characterized by the breakdown of cartilage. Effective delivery of IGF-1 to damaged cartilage is crucial for its therapeutic effects. Techniques such as intra-articular injections and localized delivery systems are being explored to ensure that IGF-1 reaches the target tissue in sufficient concentrations. Animal studies have demonstrated that continuous administration of IGF-1 can prevent cartilage degradation and promote repair, highlighting its potential as a treatment for osteoarthritis (Wen et al., 2021).
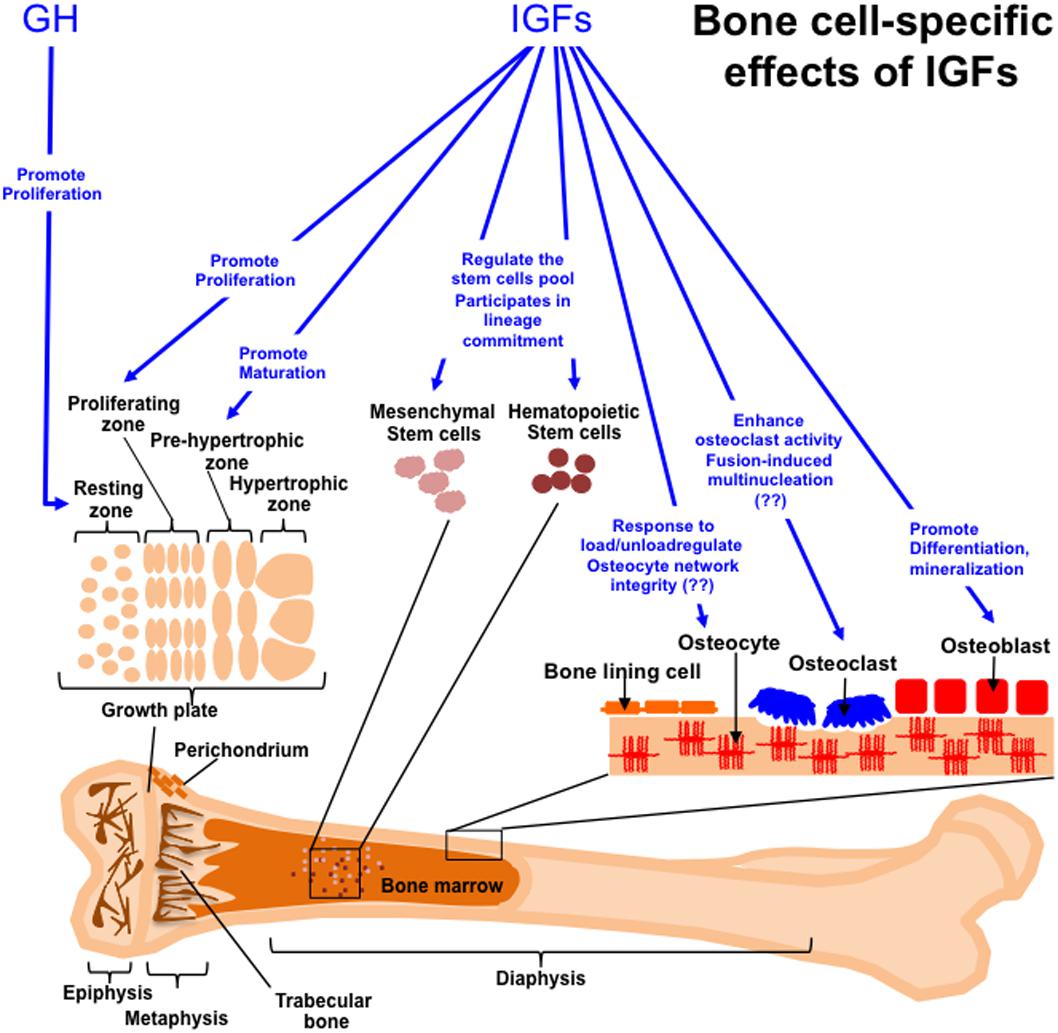
Bone Tissue
IGF-1 significantly influences bone metabolism by promoting both bone resorption and formation. This dual action is crucial for bone remodeling, a continuous process where old bone tissue is replaced by new bone tissue. IGF-1 stimulates osteoblasts, the cells responsible for bone formation, to produce new bone matrix. It also promotes the activity of osteoclasts, the cells responsible for bone resorption, to remove old or damaged bone, facilitating the replacement process (Canalis, 2009).
The effects of IGF-1 on bone health are particularly evident in conditions involving bone fractures and osteoporosis. Studies have shown that administering IGF-1 to patients with fractures can accelerate bone healing and improve clinical outcomes. For example, IGF-1 treatment has been found to increase bone mineral density and enhance the structural properties of the healed bone, making it stronger and less prone to re-injury (Locatelli & Bianchi., 2014).
In addition to its direct effects on bone cells, IGF-1 also influences bone health by interacting with other hormones, such as parathyroid hormone (PTH) and vitamin D. These interactions help regulate calcium homeostasis and ensure that bones receive adequate nutrients for growth and repair. By modulating these hormonal pathways, IGF-1 plays a critical role in maintaining bone health and preventing diseases such as osteoporosis (Canalis, 2010).
IGF-1 and Glucose Metabolism
IGF-1 has significant effects on glucose metabolism, particularly in enhancing insulin sensitivity and regulating blood glucose levels. It stimulates glucose transport into muscle cells through IGF-1 receptors or hybrid insulin/IGF-1 receptors. By increasing glucose uptake in muscle cells, IGF-1 helps lower blood glucose levels, thereby reducing the need for insulin secretion (Clemmons, 2004).
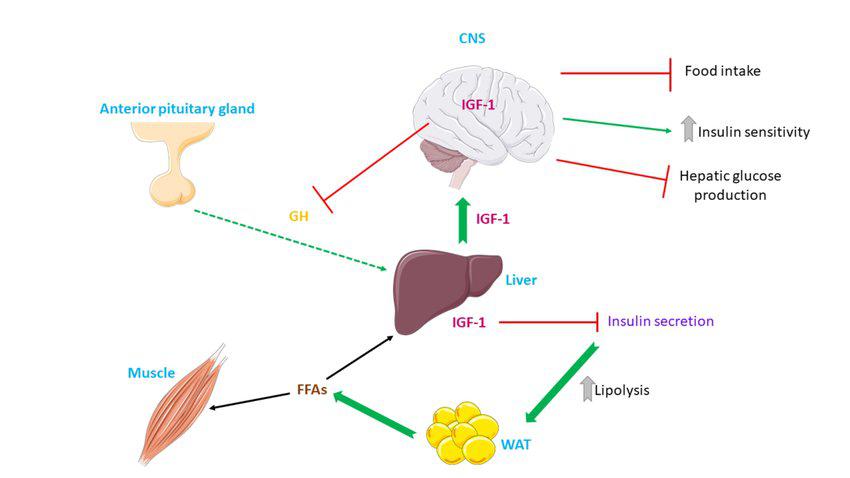
Description of the metabolic actions elicited by IGF-1. IGF-1 is released mainly from the liver and improves insulin sensitivity by suppression of insulin secretion, in turn leading to augmented lipolysis in adipose tissue and promotion of NEFA use in muscle and liver. Abbrevations used: CNS: central nervous system; GH: growth hormone; IGF-1: insulin growth factor-1; FFAs: free fatty acids; WAT: white adipose tissue
In animal models, high concentrations of free IGF-1 have been shown to inhibit gluconeogenesis, the process by which glucose is produced from non-carbohydrate sources in the liver. This inhibition helps reduce blood glucose levels and improves overall glucose homeostasis. Additionally, studies have demonstrated that removing the insulin receptor in mice decreases blood glucose levels in response to IGF-1, indicating that IGF-1 can compensate for insulin's role in glucose metabolism to some extent (Clemmons, 2004).
Clinical studies have also highlighted the importance of IGF-1 in maintaining glucose metabolism. For instance, research has shown that low levels of serum IGF-1 are associated with impaired glucose tolerance and an increased risk of type 2 diabetes. Conversely, higher levels of IGF-1 correlate with better insulin sensitivity and lower blood glucose levels. These findings suggest that IGF-1 plays a crucial role in preventing metabolic disorders and maintaining glucose homeostasis (Rajpathak et al., 2014).
IGF-1 and Aging
The IGF-1 pathway is highly conserved across various species, from invertebrates to mammals. This pathway is crucial for regulating growth, development, and lifespan. In mammals, the IGF-1 pathway involves a complex network of signals that influence cellular processes such as growth, metabolism, and aging. IGF-1 exerts its effects through the IGF-1 receptor, which activates a cascade of intracellular signaling pathways that promote cell growth and survival (Kenyon, 2010).
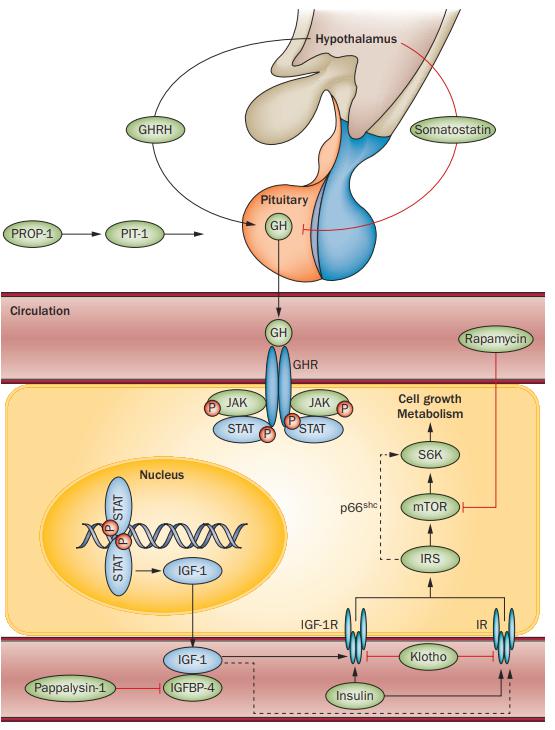
Factors of the GH/IGF-1 axis known to influence ageing. The embryonically expressed genes PROP1 (which encodes PROP-1) and POU1F1 (which encodes PIT-1) are involved in pituitary development, including differentiation of pituitary somatotrophic cells.
If there is one insulin/IGF-1 pathway in invertebrates, in higher vertebrates, including mammals, this pathway is divided into two. These two pathways have overlapping functions, but insulin is mainly involved in the regulation of metabolism, and the Growth Hormone/IGF-1 pathway plays an important role in the processes of growth, development and possibly life expectancy. It was the IGF-1 cascade genes that became the first discovered "aging genes" — that is, genes whose damage led to an increase in life expectancy.
In humans, variations in IGF-1 levels and signaling have been linked to aging-related diseases. Low IGF-1 levels are often associated with increased risk of cardiovascular diseases, diabetes, and neurodegenerative disorders. Conversely, higher IGF-1 levels are linked to better health outcomes and reduced risk of these conditions. These findings highlight the importance of IGF-1 in promoting healthy aging and preventing age-related diseases (Kenyon, 2010).
Effects on the Skin
IGF-1 plays a crucial role in maintaining skin health and promoting wound healing. It acts as a regulator and stimulator of cell division in epithelial tissue, enhancing the growth and metabolism of cells in the deeper layers of the skin. This leads to accelerated collagen synthesis and faster healing of both superficial and deep wounds. IGF-1 also plays a key role in maintaining epidermal homeostasis, helping to prevent skin aging and maintain a youthful appearance (Tavakkol et al., 1999).
The mechanism by which IGF-1 promotes skin health involves several cellular processes. When skin is injured, IGF-1 stimulates the proliferation of keratinocytes, the primary cells in the epidermis, and fibroblasts, the cells responsible for producing collagen and other extracellular matrix components. This increased cell proliferation and matrix production help repair the damaged skin and restore its structural integrity. Additionally, IGF-1 enhances the migration of these cells to the wound site, further accelerating the healing process (Zhang et al., 2024).
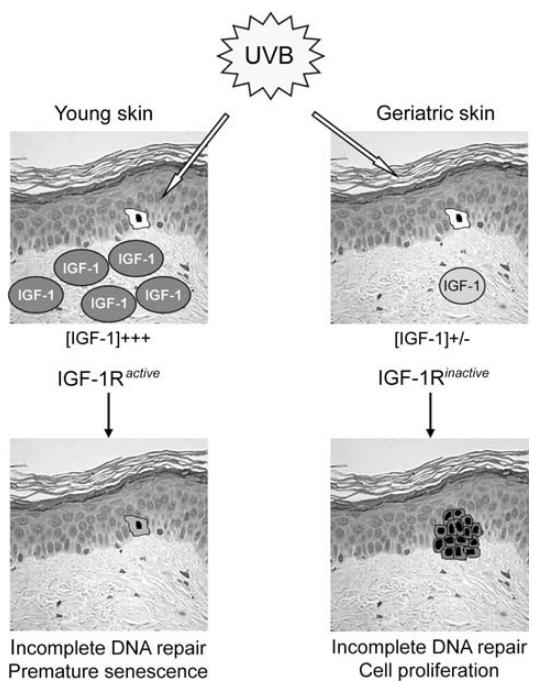
The influence of aging on insulin-like growth factor 1 (IGF-1) expression in the skin and its role in ultraviolet-B (UVB)- induced carcinogenesis.
Studies have shown that IGF-1 can also protect the skin from the effects of aging. By promoting collagen synthesis and reducing the breakdown of collagen fibers, IGF-1 helps maintain skin elasticity and firmness. This anti-aging effect is particularly important for preventing the formation of wrinkles and maintaining a smooth, youthful complexion. Furthermore, IGF-1 has been found to reduce inflammation in the skin, which can help prevent chronic skin conditions and improve overall skin health (Muraguchi et al., 2019).
Effects on Nerve Tissue
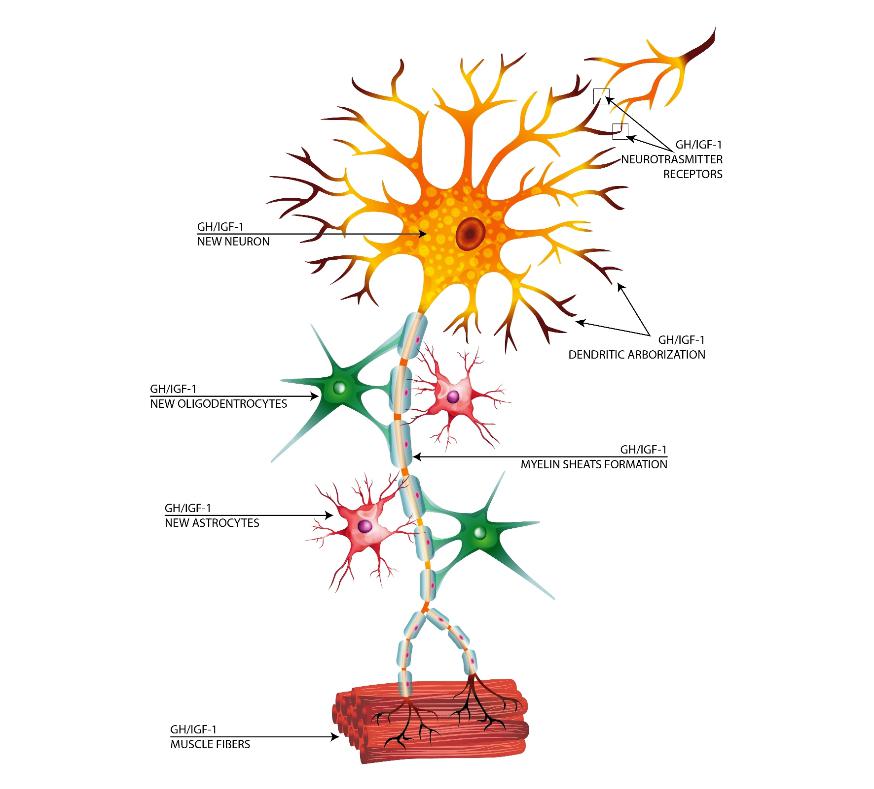
IGF-1 has significant neuroprotective effects, enhancing the survival and function of neurons. It increases glucose transport into neurons, providing them with the energy needed for proper functioning. This is particularly important in conditions of low glucose levels, where IGF-1 helps prevent neuronal damage and cell death. Additionally, IGF-1 stimulates the synthesis of neuronal RNA and promotes the formation of axons, the long projections of neurons that transmit nerve signals (Dyer et al., 2016).
In the nervous system, IGF-1 also enhances the proliferation of glial cells, which provide support and protection for neurons. These glial cells include astrocytes, oligodendrocytes, and microglia, each playing a crucial role in maintaining the health and function of the nervous system. By promoting the proliferation and function of these cells, IGF-1 helps create a supportive environment for neurons, facilitating their growth, repair, and survival (Carson et al., 1993).
IGF-1's neuroprotective effects are particularly relevant in neurodegenerative diseases such as Alzheimer's and Parkinson's disease. Research has shown that IGF-1 can reduce the accumulation of toxic proteins, such as beta-amyloid plaques in Alzheimer's disease, and enhance the clearance of these proteins from the brain. This helps protect neurons from damage and supports cognitive function. Additionally, IGF-1 has been found to promote the regeneration of damaged neurons, offering potential therapeutic benefits for neurodegenerative conditions (Dyer et al., 2016).
Effects on the Cardiovascular System
IGF-1 plays a specialized role in cardiovascular health by promoting the development and function of the heart and blood vessels. It enhances cardiac output, stroke volume, contractility, and ejection fraction, all of which are crucial for maintaining efficient heart function. IGF-1 also stimulates the remodeling of heart tissue, helping to repair damage after myocardial infarction and improve overall cardiac health (Macvanin et al., 2023).
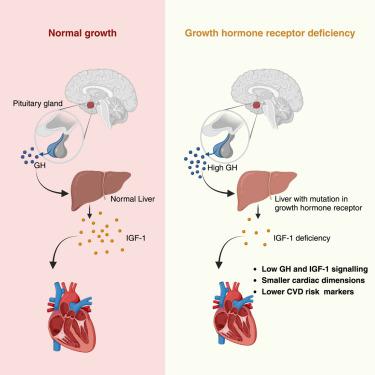
The cardiovascular effects of IGF-1 are mediated through several mechanisms. First, IGF-1 promotes the proliferation and survival of cardiomyocytes, the muscle cells of the heart. This helps maintain the structural integrity and contractile function of the heart. Second, IGF-1 stimulates angiogenesis, the formation of new blood vessels, which improves blood flow and oxygen delivery to the heart and other tissues. Third, IGF-1 has anti-apoptotic and anti-inflammatory effects, reducing cell death and inflammation in the cardiovascular system (De Giorgi et al., 2022).
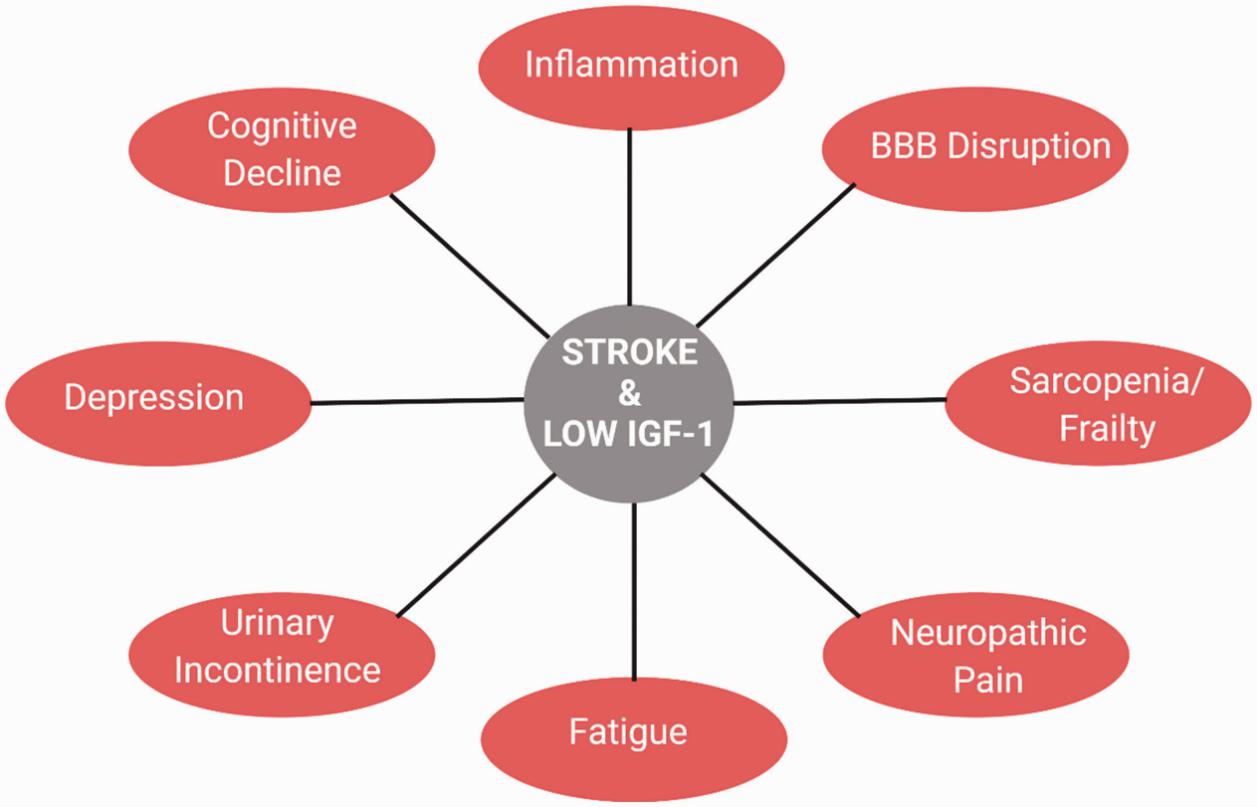
Clinical studies have shown that low levels of IGF-1 are associated with an increased risk of cardiovascular diseases, including coronary heart disease and stroke. Conversely, higher levels of IGF-1 are linked to better cardiovascular health and reduced risk of these conditions. For example, a prospective cohort study patients found that participants with higher IGF-1 levels had a 55% lower relative risk of myocardial infarction compared to those with lower levels (Macvanin et al., 2023).
Effects on Immunity
IGF-1 has a significant impact on the immune system, enhancing the function and proliferation of various immune cells. It increases the populations of T-lymphocytes, B-lymphocytes, and natural killer cells, all of which play crucial roles in the body's defense against infections and diseases. IGF-1 also enhances the activity of T-lymphocytes, which are essential for cell-mediated immunity and the destruction of infected or cancerous cells (Alpdogan et al., 2003).
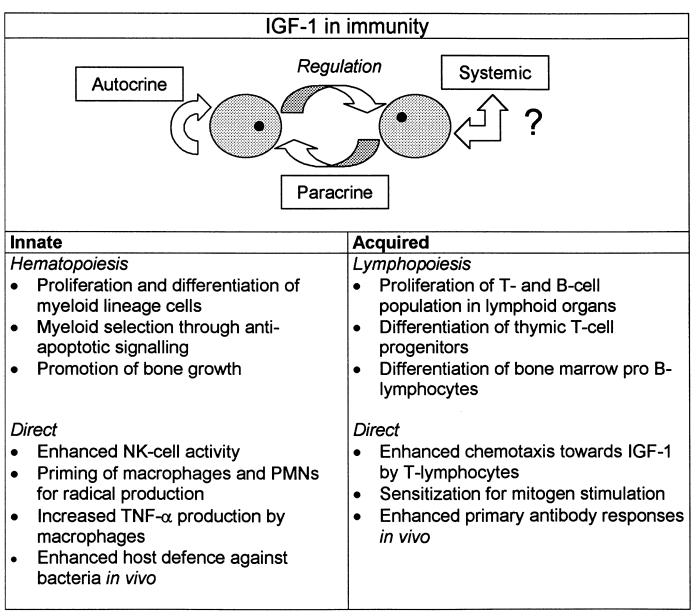
The immune-enhancing effects of IGF-1 are mediated through several mechanisms. IGF-1 stimulates the proliferation of immune cells by binding to its receptors on their surface, leading to increased cell division and growth. This is particularly important for the expansion of immune cell populations in response to infections or immunological challenges. Additionally, IGF-1 enhances the function of these cells by promoting their activation and increasing their ability to respond to pathogens (Dyer et al., 2016).
Research has shown that IGF-1 can also protect immune cells from apoptosis, or programmed cell death, which is crucial for maintaining a robust immune response. For example, studies have demonstrated that IGF-1 can inhibit the apoptosis of macrophages and neutrophils, two key types of immune cells involved in the body's initial response to infection. By preserving the viability of these cells, IGF-1 helps ensure an effective and sustained immune response (Alpdogan et al., 2003).
APPLICATION OF IGF-1 LR3
IGF-1 LR3is often the secret weapon of professional bodybuilders. It is the use of this product that is the next step for progress after anabolic steroids and growth hormone, which have long gained popularity among the world of PEDs lovers.
The IGF-1 LR3 product is very broad-acting and can be used both for fat burning, acceleration of injury healing and strengthening of the articular-ligamentous apparatus, gaining muscle mass and accelerated recovery after exertion, because the substance also affects the recovery of the nervous system. IGF-1 LR3 software has a rich range of properties that are suitable for many purposes and will be an excellent addition to any of your courses, whether it is a set of muscle mass or pre-competitive training.
Dosage:
Beginners: 20-40 mcg per day
Intermediate: 40-60 mcg per day
Advanced: 60-100 mcg per day
Cycle Duration:
Typically, 4-6 weeks, followed by a break of equal length to avoid desensitization.
Administration Schedule:
Frequency: Daily injections
Timing: Administered in the morning or post-workout to maximize absorption and effectiveness.
Injection Site: Subcutaneous or intramuscular injections, rotating sites to prevent tissue damage.
Example
| Timeframe (weeks) | Daily IGF-1 LR3 dosage |
|---|---|
| 1-6 | 20-100 mcg (consider initiating at lower dose to assess tolerance) |
| 7-12 | Washout |
| 13-18 | 20-100 mcg |
| 19-24 | Washout |
After injection of IGF-1 LR3 (insulin-like growth factor 1, long variant), the concentration in the blood reaches a peak after about 1-2 hours. The effects can persist for 24-30 hours, as IGF-1 LR3 has a longer half-life compared to conventional IGF-1
Overdose
Overdose can cause the side effects that are listed above. Most often, this is hypoglycemia – a decrease in sugar below the 3.5 mmol/l mark. In this case, it is necessary to eat a certain amount of carbohydrate food until the condition stabilizes.
Method of administration
Intramuscular or subcutaneous injections using insulin syringes.
Detection during doping tests
If you stop taking the drug three days before testing, no one will be able to detect the substance in the blood.
Potential risks
Among fans of PEDs, there is information that links IGF-1 with the development of cancer. Although this supposed correlation has a great impact on the mass media, most clinical and epidemiological reports to date have not revealed a causal relationship between growth hormone therapy and as a consequence of an increase in IGF-1 levels and an increased risk of cancer (Werner & Laron., 2020).
Based on these data, the IGF-1 drug itself does not cause oncology, but only has a contraindication to use if you already have cancer or its predisposition (high cancer markers). Growth hormone and IGF-1, even in high pharmacological doses, are not able to induce malignant transformation. However, the GH-IGF1 axis is able to "push" already transformed cancer cells through various phases of the cell cycle.
HOW TO USE IGH-1 LR3
All peptide hormones in our product line (except for liquid growth hormone) are lyophilized. Peptides supplied as lyophilized powder come with a solvent (bacteriostatic water in a 1 ml ampoule). This solvent is used to prepare a solution, which will then be stored in liquid form.
Ampoule with Solvent (Bacteriostatic Water)
In an aqueous environment, peptides degrade quickly. This is partly due to the presence of bacteria, for which water provides an ideal environment for growth and reproduction. The injection water is sterile. However, once the package (usually an ampoule or vial) is opened, sterility is compromised. To maintain sterility for as long as possible, benzyl alcohol or metacresol is added for their strong antibacterial properties. This treated water is called bacteriostatic, meaning bacteria remain in a "static state" and do not reproduce. Growth hormone and other peptides in a bacteriostatic environment can maintain their stability and resist degradation for much longer.
How to Prepare the Solution
- Fill the syringe with water. Typically, the vial contents are dissolved in one milliliter of water.
- Add water to the vial containing the lyophilized powder. Tilt the vial so the needle touches the vial wall.
- Avoid letting the diluent contact the freeze-dried powder directly. The diluent should flow slowly down the sides of the vial (do not pour it all at once and avoid rushing).
- Once all the solvent has been added to the vial with the peptide, gently swirl (but do not shake) the vial until the lyophilized powder dissolves and you obtain a clear liquid. The solution is now ready for use.
- Store the prepared solution at a temperature of 2-8°C.
Watch the video how to prepare the solution ⤵️
https://t.me/driadaeducation/52
Syringes for Injection

It is recommended to use syringes that are fresh out of the package to prevent infection (reusing syringes increases the risk of infection). Insulin syringes are typically used for subcutaneous injections and can have either a removable needle or a fixed needle. One of the most popular injection needles is the G30. Syringes usually come in 1 ml and 0.5 ml sizes.
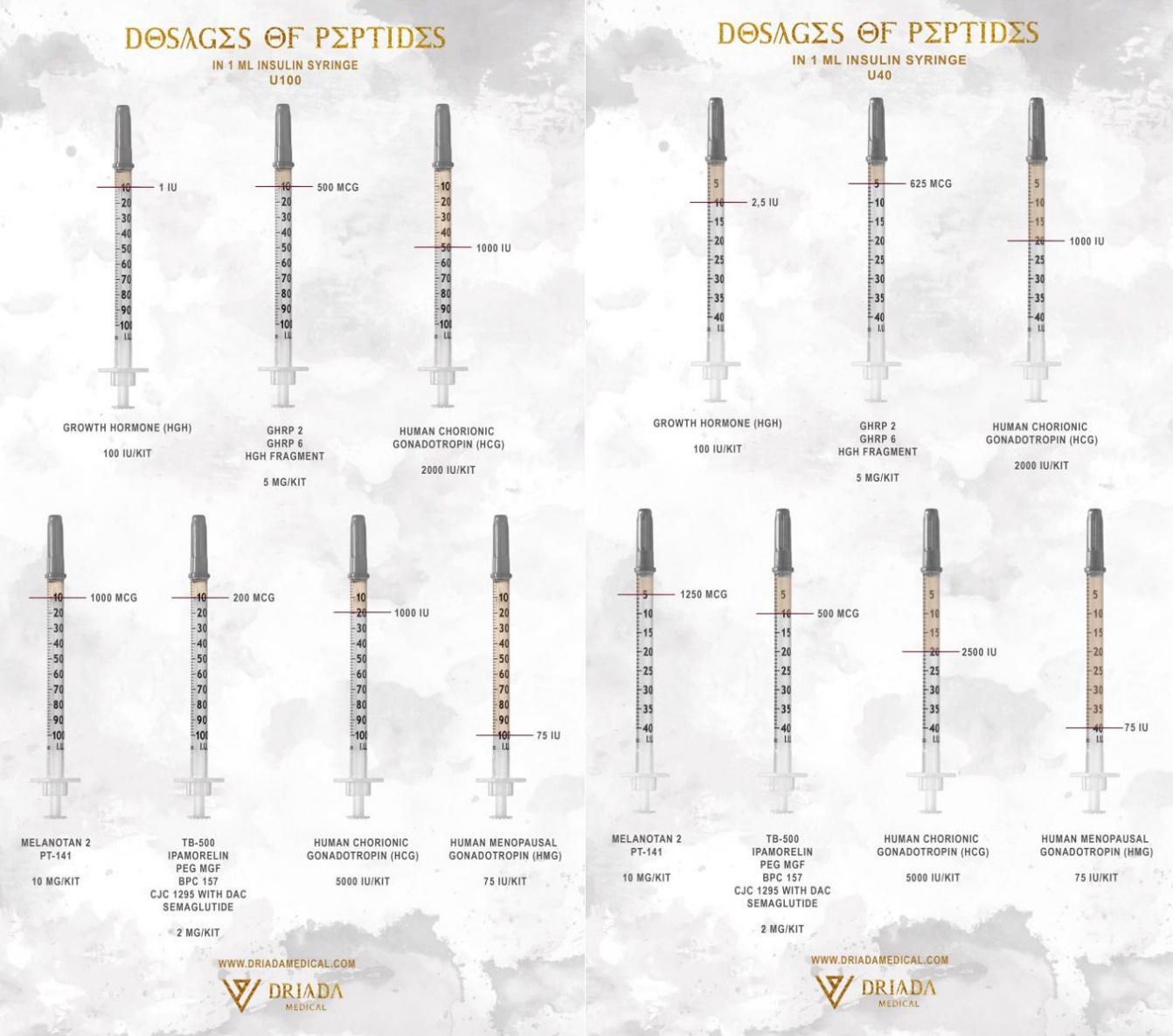
Insulin syringes come in U40 and U100 formats, which correspond to the insulin content of 40 units per 1 ml and 100 units per 1 ml, respectively. Each syringe is specifically designed for a particular type of insulin. However, this does not apply to units of growth hormone or mg of peptides, so both types of syringes can be used with appropriate adjustments to determine the correct dosage. These syringes have different markings, and by referring to these markings, you can determine the number of units of growth hormone to inject. Below, we provide a picture showing the dosage of various peptides when mixed with 1 ml of water for U100 and U40 syringes.
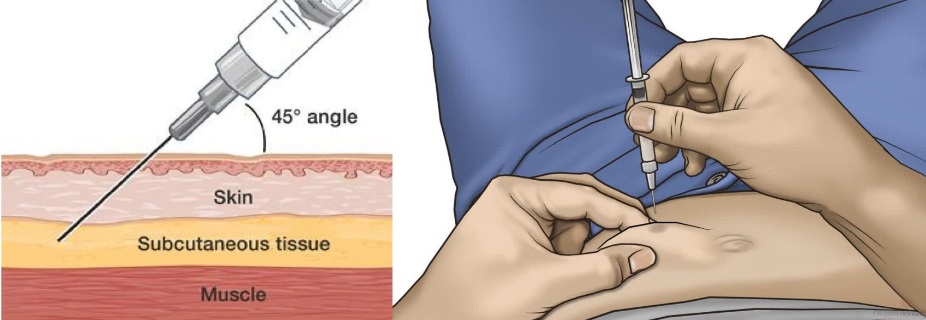
Subcutaneous Injections
After diluting the peptide with water, it is ready for use. All peptides are injected subcutaneously or intramuscularly using an insulin syringe.
You will need:
- Alcohol swab
- Insulin syringe
- Bottle with the prepared solution
Injection Procedure:
- Remove the bottle cap.
- Wipe the rubber stopper of the bottle with alcohol.
- Take an insulin syringe and insert it into the bottle.
- Draw the required amount of solution into the syringe.
- Wipe the injection site with an alcohol swab.
- Hold the needle at a 30-45 degree angle and inject.
- Inject the solution slowly.
- After finishing, hold the needle in place for 10 seconds before removing it to prevent leakage of the injected liquid.
- Synergistic increase in muscle mass
- Synergistic effect of fat burning
- Strengthening the action of anabolic steroids
- Synergistic effect on strengthening bone tissue
- Synergistic increase in muscle mass
- Synergistic effect of fat burning
- Synergistic effect on tendon repair
- Synergistic effect on strengthening bone tissue
- Increased risk of side effects from excessive IGF-1 levels
- Synergistic increase in muscle mass
- Increased risk of hypoglycemia
Storage
Proper storage of peptide drugs is crucial to maintaining their effectiveness. Below are the guidelines for storing peptides in various forms.
Storage of the Powder Form
The powder form (unmixed) can be stored at room temperature or in the refrigerator. Lyophilized powder should be kept away from direct sunlight and excessive heat. Under appropriate storage conditions, peptides in dry form can be stored for up to 3 years at 2-8°C and up to 2 years at 15-30°C. If the vial is damaged and air gets inside, the active substance will decompose quickly outside the refrigerator, retaining only about half of its concentration within two weeks. Therefore, if the packaging's integrity is uncertain, it is best to store the peptide in the refrigerator.
Storage of Bacteriostatic Water
Bacteriostatic water should always be stored in the refrigerator at 2-8°C to maintain its properties. If the peptide and bacteriostatic water are stored together, keep the entire set in the refrigerator.
Storage of the Solution
After mixing the powder with water from the ampoule, the peptide solution must be stored in the refrigerator. Without refrigeration, the peptide begins to degrade, and within a few days, the molecules will break down completely. The storage duration for each peptide varies. For instance, growth hormone can be stored in the refrigerator for only 2-3 days, while HCG can last about 5 weeks. On average, other peptides can be stored for at least 30 days, though some may last even longer. The degradation rate also depends on the number of bacteria introduced when piercing the vial, which is unavoidable to some extent.
!!! NEVER STORE PEPTIDES IN THE FREEZER !!!
Use with anabolic steroids
It is also perfectly appropriate to use IGF-1 with anabolic steroids and other drugs with similar effects. IGF-1-1 enhances the effects of anabolic steroids by increasing the number of androgen receptors. The drug IGF-1 is an extremely powerful anabolic that, in combination with AS, gives a very large increase in lean muscle mass. At the same time, IGF-1 has a lot of other useful properties that together create the maximum background for growth.
All anabolic steroids act on muscles through special structures – receptors. There is an opinion that if you use steroids for a long time, the number of these receptors decreases. The number of these receptors also decreases with age. In this case, it becomes necessary to use large doses of steroids. In 20 years, 300 mg of testosterone Propionate acts more powerfully than in 30 years. At 30 years of age, 600 mg is needed for the same effect. IGF-1 activates cells and increases the number of androgen receptors, and at 30 years of age, then 300 mg of testosterone propionate will act the same as at 20 years of age.
Effects
Use with Growth Hormone (Somatropin)
The use of somatotropin at the same time may be advisable, although it may not seem logical at first glance, nevertheless, many professional bodybuilders do just that. When used together, their effects add up – as an anabolic effect for muscle growth, and for the restoration and regeneration of cartilage and other collagen structures. Also, growth hormone and IGF-1 together will increase fat burning.
It should be borne in mind that in addition to beneficial effects, the presence of side effects may also occur. It should be understood that the level of IGF when using both drugs will increase significantly, so such use should not be prolonged.
Effects
Use with insulin
As the name IGF-1 implies, it has a structure similar to insulin, and binds not only to its own IGF1R receptor, but also to the insulin receptor — and vice versa. However, the binding affinity for IGF1R and the insulin receptor, respectively, is different, with a high affinity of IGF-1 for IGF1R and about 10 times lower affinity for the insulin receptor.
On the other hand, the affinity of insulin to its own receptor is about 100 times higher compared to IGF1R. Moreover, despite the similarity in structure, IGF-1 and insulin show different distribution in tissues, different internalization kinetics and different subcellular distribution of hormonal receptors. Consequently, both hormones can affect similar pathways, but to different degrees, and, in addition, differentially activate other pathways located downstream.
These hormones can be compared in the plane of the effect on glucose metabolism in the body. When they are used together, such a side effect as hypoglycemia (a drop in sugar levels) will be so pronounced that it will create risks to life.


